Unbelievable Cancer Breakthrough: Bacteria That Shrink Tumors Without Immune Help!

Imagine a world where tiny bacteria could be the key to shrinking tumors without relying on the body’s immune system! A groundbreaking study from Japan reveals just that, showcasing an innovative therapy that offers hope for those weary of traditional cancer treatments.
Seigo Iwata from the Japan Advanced Institute of Science and Technology (JAIST) is leading this thrilling research. His team has found that a special combination of bacteria can be administered intravenously, leading to remarkable tumor remission without triggering harmful side effects like cytokine release syndrome (CRS).
So, what’s the secret sauce? This therapy utilizes two unique species of bacteria: Proteus mirabilis, referred to as A-gyo, and Rhodopseudomonas palustris, known as UN-gyo. These bacteria work in harmony, initially delivered in a stable ratio that transforms inside the tumor, ramping up the anti-cancer effects where they matter most.
A-gyo is no ordinary strain; it’s been engineered to avoid pathogenic properties that could harm the body, allowing it to thrive within tumors safely. Meanwhile, UN-gyo acts as a regulator, controlling A-gyo's actions while enhancing its potency against cancer cells.
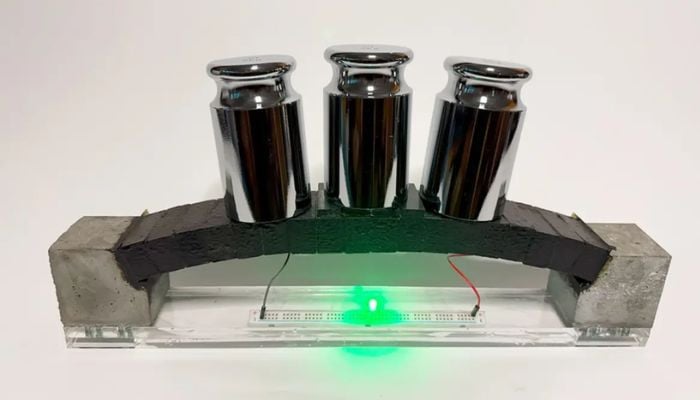
The initial mix is about 3% A-gyo and 97% UN-gyo, but don’t let that ratio fool you! Inside the tumor environment, these bacteria flip the scales, with A-gyo making up to 99% as it decimates tumor cells. The results are stunning: tumors darken and shrink as blood clots form within their vessels, leading to localized vascular collapse.
This innovative therapy is particularly significant for patients undergoing chemotherapy or radiation, as these treatments often leave individuals immunocompromised. Unlike conventional therapies that depend on immune responses, this bacterial duo can operate independently of the immune system's health.
In studies, a single intravenous dose of A-gyo and UN-gyo rapidly shrank tumors, and a two-dose regimen led to complete responses in various mouse models. This included human tumor xenografts like colorectal, ovarian, and pancreatic cancers, showcasing the therapy’s vast potential.
But there are still challenges ahead. While the bacteria showed no systemic toxicity at effective doses, researchers must navigate the fine line of dosing. High doses did result in complications, indicating a need for careful management of treatment protocols.
As this study demonstrates, the world of cancer treatment is evolving. The potential of using bacteria as a therapeutic agent highlights a fascinating avenue of research that could reshape how we approach cancer therapy.
With plans for extensive testing and human trials on the horizon, the future of cancer treatment may very well lie in the microscopic world of bacteria—opening doors to possibilities we once only dreamed of.
This remarkable study was published in Nature Biomedical Engineering, and it’s only the beginning of what could be an extraordinary journey in the fight against cancer.