Singapore Researchers Launch Groundbreaking Stem Cell Trial for Parkinson’s Disease
In an exciting development for neuroscience, researchers from Singapore's National Neuroscience Institute (NNI) are set to embark on a pioneering project aimed at transplanting stem cells into the brains of patients diagnosed with early-stage Parkinson’s disease. This innovative clinical trial seeks to halt the progression of this debilitating condition, which affects thousands in the region.
The groundwork for this unprecedented trial is currently under preparation, with researchers awaiting necessary regulatory and ethical approvals before they can proceed. If all goes as planned, the phase one trial could commence as early as late 2026. The initial phase will involve five to eight younger patients who are experiencing complications from their existing treatments.
This ambitious project is being supported by a substantial funding boost of $25 million, granted by the National Medical Research Council on May 28. This funding is allocated over a five-year period under a program known as the Singapore Parkinson’s Disease Programme, or SPARKLE, which aims to explore various aspects of Parkinson’s disease.
Parkinson’s disease currently affects an estimated 8,000 individuals in Singapore alone. This neurodegenerative disorder arises when dopamine-producing neurons in the brain progressively deteriorate. As dopamine levels diminish, patients experience a range of symptoms, including tremors, rigidity, and slowed movements. Unfortunately, there is no cure available for this condition, which complicates basic activities related to walking, balance, coordination, and even speech.
The concept of utilizing stem cells to replace the brain cells lost to Parkinson’s has been a topic of research for the past four decades. The goal is for these transplanted stem cells to develop into dopamine-producing neurons, potentially reversing the symptoms of the disease. However, previous attempts have faced numerous challenges, including ethical concerns regarding the use of stem cells derived from embryos and inconsistent outcomes, where some transplanted cells did not yield dopamine and sometimes caused undesirable side effects, such as involuntary movements.
Advancements in cellular therapy have led to significant progress in this field. Researchers are now able to transform a patient's own normal body cells—such as those obtained from skin or blood—into stem cells. This technique minimizes the risk of the body’s immune system rejecting the transplanted cells, making it a promising avenue for treatment.
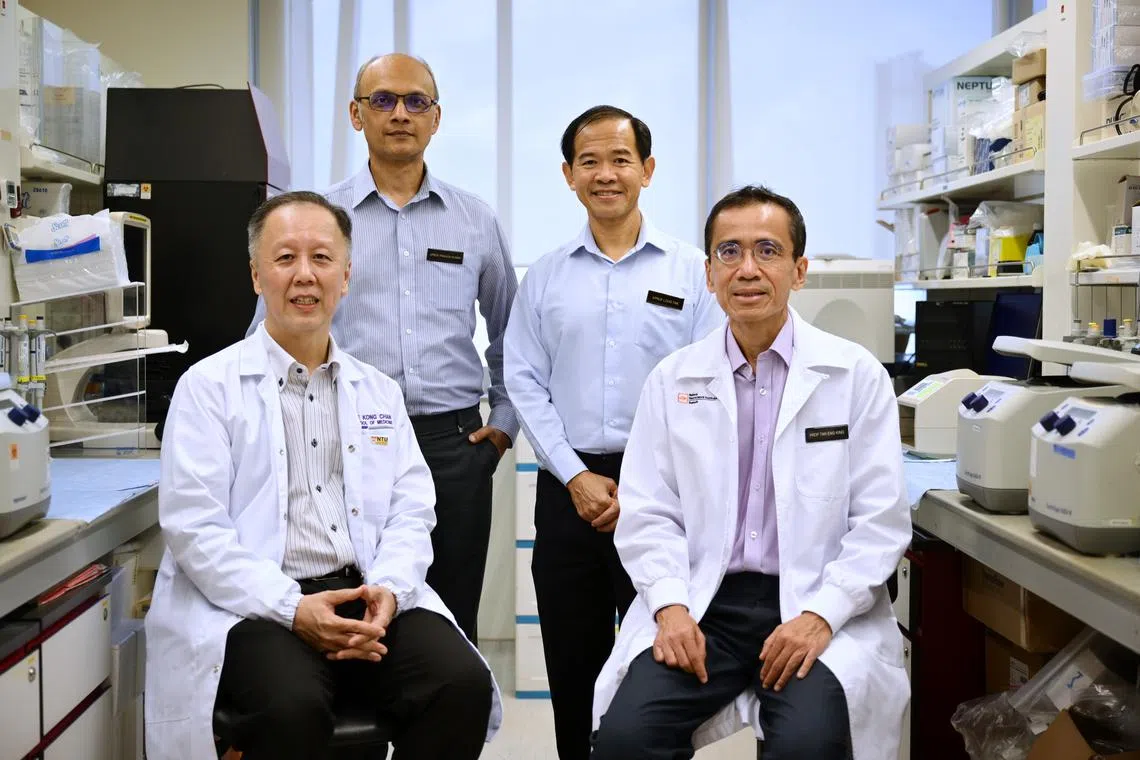
Professor Tan Eng King, the principal investigator for the SPARKLE initiative and deputy CEO for academic affairs at NNI, stated that the institute has collaborated with esteemed institutions, including Duke-NUS Medical School, Lee Kong Chian School of Medicine, and A*Star, to create a proprietary method to convert normal cells into stem cells. The therapy is currently undergoing final approval processes by the U.S. Food and Drug Administration before it can proceed to the trial stage.
Moreover, other researchers worldwide are exploring similar stem cell therapies to tackle Parkinson’s disease. According to Professor Tan, the group that succeeds in creating a stem cell source featuring nearly 100 percent dopamine-producing cells will lead the way in this research field. He emphasized the complexity of this endeavor, stating, “This is a very challenging endeavor and it is not something that anybody can do. We have developed the expertise, and we think that potentially, we can be one of the pioneers.”
Following the stem cell transplant, participants in the trial will be monitored for approximately two years to assess both the safety and efficacy of this new treatment approach.
In addition to the stem cell trial, the SPARKLE program also includes a community-based early screening initiative aimed at identifying individuals who are at high risk of developing Parkinson’s disease. Professor Tan expressed optimism that this screening program could be launched by the end of 2025, targeting about 10,000 individuals aged 55 and above over the next three to five years.
Currently, Singapore lacks a reliable screening method for early detection of Parkinson’s disease. However, previous research conducted by NNI indicates that certain warning signs—such as a diminished sense of smell, rapid eye movement sleep disorder (a condition where individuals act out their dreams), and specific genetic variants—may correlate with a higher likelihood of developing the disease.
The screening process will involve a comprehensive questionnaire, and those who score at risk will be invited for detailed examinations, including brain scans. Individuals identified as at high risk will receive tailored interventions aimed at mitigating their risk, which may involve lifestyle modifications encompassing dietary changes and increased physical activity.
Professor Tan highlighted that Singapore boasts one of the highest life expectancies globally, and reducing the risk of developing neurodegenerative conditions like Parkinson’s could significantly enhance the quality of life for many citizens. “If you can reduce the risk of developing a neurodegenerative condition, then you can increase the amount of years that you can spend in healthier living,” he stated.
Stay updated with the latest news by joining ST's WhatsApp Channel.