Wes Streeting Discusses £1bn Redundancy Payouts Amid NHS Overhaul

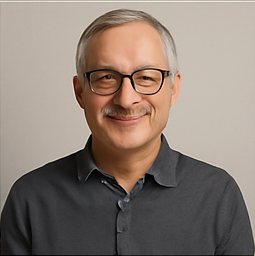
In a recent session before the health and social care select committee, Health Secretary Wes Streeting acknowledged that the cost of redundancy payouts across the National Health Service (NHS) in England could reach £1 billion, a figure he deemed a “reasonable ballpark” for the financial implications of staffing cuts. This admission comes on the heels of a significant governmental restructuring that involves the dissolution of NHS England, an entity that previously employed over 15,000 individuals. The government has asserted that this move is aimed at not only saving money but also restoring democratic oversight to the management of the health system.
The announcement of NHS England's abolition was met with a mix of concern and cautious optimism, as the government has laid out plans for NHS trusts to curtail their “corporate cost growth.” In addition, integrated care boards have received directives to slash their operational costs by 50% starting in October. These measures are part of a broader strategy to streamline operations within the NHS to make it more efficient.
According to accounts from the Department of Health, the average redundancy package for employees across the NHS and its associated agencies was reported to be approximately £48,840 for the fiscal year ending in March 2024. However, recent reports from The Observer suggest that the latest wave of staff exits could incur costs as high as £1.2 billion, prompting critical discussions among health leaders and stakeholders about the financial impact of these cuts.
When pressed by committee members about the potential costs of redundancy and how they would be financed, Streeting expressed confidence in justifying the expenditure by highlighting the long-term savings that could result from a reduced workforce. “I didn’t think that was an unreasonable ballpark figure, and I would justify that cost on the basis of the fact we will more than pay for that in terms of the savings that are achieved year on year,” he stated, emphasizing the necessity of strategic planning in managing NHS resources.
However, he also noted that precise figures regarding the overall cost of redundancies would not be available until the Department of Health has finalized plans regarding the restructured organization, including its size and the exact number of staff affected. Health leaders have been vocal in calling for the establishment of a dedicated “redundancy fund” that would support NHS organizations as they navigate these substantial cuts to their workforce.
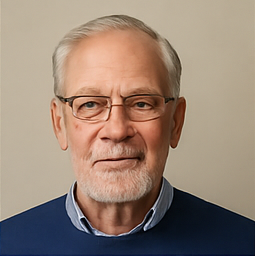
In a related inquiry about how the redundancy bill would be financed, Sir James Mackey, the interim chief executive of NHS England, indicated that discussions with the Treasury are already underway. “We have just started a discussion with the Treasury about how the redundancy costs are managed, but that’s not complete yet,” Mackey informed the committee, indicating that the future funding structure remains uncertain.
When asked if the funds required for these redundancy payouts would come from the current health budget, Streeting clarified that any decisions would be “subject to discussion with the Treasury, whose servant I am.” The ongoing dialogue with the Treasury will undoubtedly be critical in determining the financial landscape for the NHS as it embarks on this significant transformation.