Unexpected Complications After Kidney Transplant: A Case Study

Approximately two months following a kidney transplant, a 61-year-old man found himself back in the hospital due to a series of alarming symptoms. Initially, he experienced fatigue, nausea, and vomiting. Additionally, he exhibited excessive thirst and produced an abnormal amount of urine, which raised immediate concerns among the medical professionals monitoring his recovery. Over the course of the next ten days, his condition deteriorated significantly. His blood oxygen levels began to plummet, his lungs filled with fluid, and he became increasingly unable to keep food down. To address his nutritional needs, doctors made the decision to insert a feeding tube. As time progressed, his blood pressure also started to fall, leading to his admission into the intensive care unit (ICU), where he was placed on mechanical ventilation. Despite the intensive care, his health continued to spiral downward.
In light of this alarming situation, the patient was transferred to the ICU at Massachusetts General Hospital, the very location where he had received the kidney transplant. At this stage, he was diagnosed with acute respiratory failure and shock, a serious combination of conditions that posed a significant threat to his life.
In a detailed case report published in this week's issue of the New England Journal of Medicine, the medical team at Mass General elaborated on their investigative approach to diagnosing the man's critical condition. Their initial steps included gathering comprehensive information about the man's symptoms from his wife, reviewing his family medical history, and reaching out to the regional organ-procurement organization that had facilitated the kidney transplant.
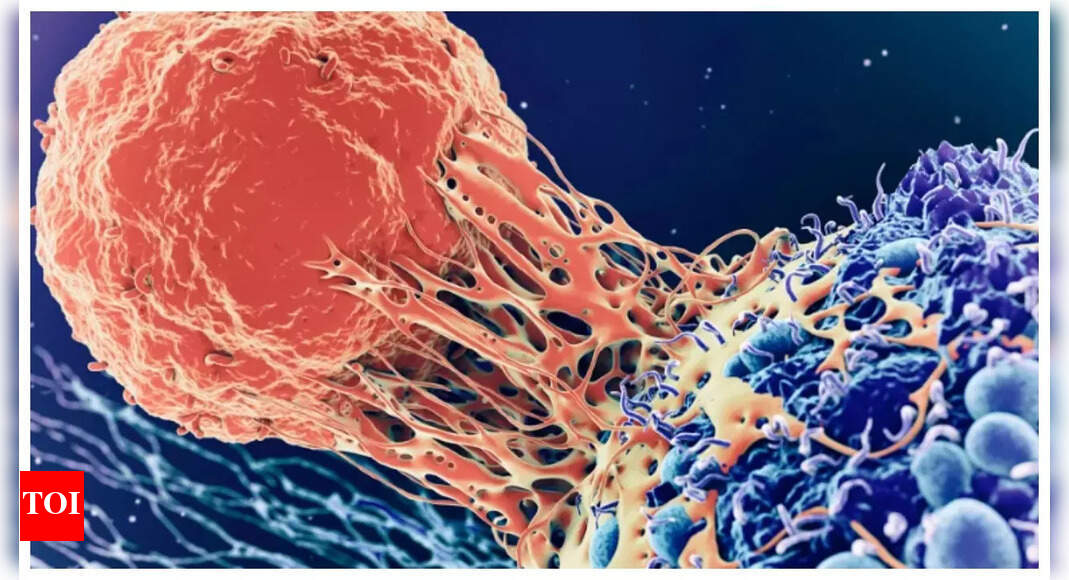
The combination of his symptoms and laboratory diagnostics suggested that the man was likely suffering from some form of infection. However, as a transplant recipient who was dependent on a regimen of immunosuppressive medications, the range of potential infections that could be causing his symptoms was quite extensive.
Dr. Camille Kotton, the Clinical Director of Mass General's Transplant and Immunocompromised Host Infectious Diseases division, outlined her methodical reasoning in working towards a diagnosis. She embarked on a careful process of elimination. The immunosuppressive drugs the patient was taking were designed to preemptively protect him against infections, effectively ruling out common culprits like herpesviruses and cytomegalovirus. Moreover, the patient was on a specific combination of antibiotics that excluded many bacterial infections and also the fungal infection Pneumocystis jirovecii, as well as the protozoan parasite Toxoplasma gondii.
However, one detail stood out prominently: the patient had developed elevated levels of eosinophils. These white blood cells can increase for various reasons, including certain parasitic infections. Compounding the situation was the presence of a reddish-purple rash on his abdomen. Given the severity of his illness, Dr. Kotton turned her focus to the possibility of a widespread parasitic infection.
As part of his medical history, it was noted that the man had been in contact with domestic cats and dogs, including a recent cat scratch he received between the time of his transplant and the onset of his critical illness. Nevertheless, common bacterial infections associated with cat scratches were ruled out. Additionally, other parasitic infections typically linked to domestic animals in the United States, like toxocariasis, do not generally lead to life-threatening conditions.