FDA Approves First Blood Test for Alzheimer’s Diagnosis
WASHINGTON (AP) — In a groundbreaking development for Alzheimer’s care, U.S. health officials announced on Friday their endorsement of the first-ever blood test designed to assist with the diagnosis of Alzheimer’s disease. This innovative test not only aids in diagnosing the condition but also identifies patients who may benefit from medications that can moderately slow the progression of this memory-destroying disease.
The test offers a crucial advantage in differentiating whether a patient’s memory issues stem from Alzheimer’s or from various other medical conditions that might also lead to cognitive difficulties. The Food and Drug Administration (FDA) has specifically approved this test for patients aged 55 and older who exhibit early signs of Alzheimer’s, marking a significant step forward in diagnostic capabilities.
Alzheimer’s disease affects over 6 million individuals in the United States alone and millions more internationally, making it the most prevalent form of dementia. The introduction of this blood test is particularly timely, given the rising prevalence of the disease worldwide.
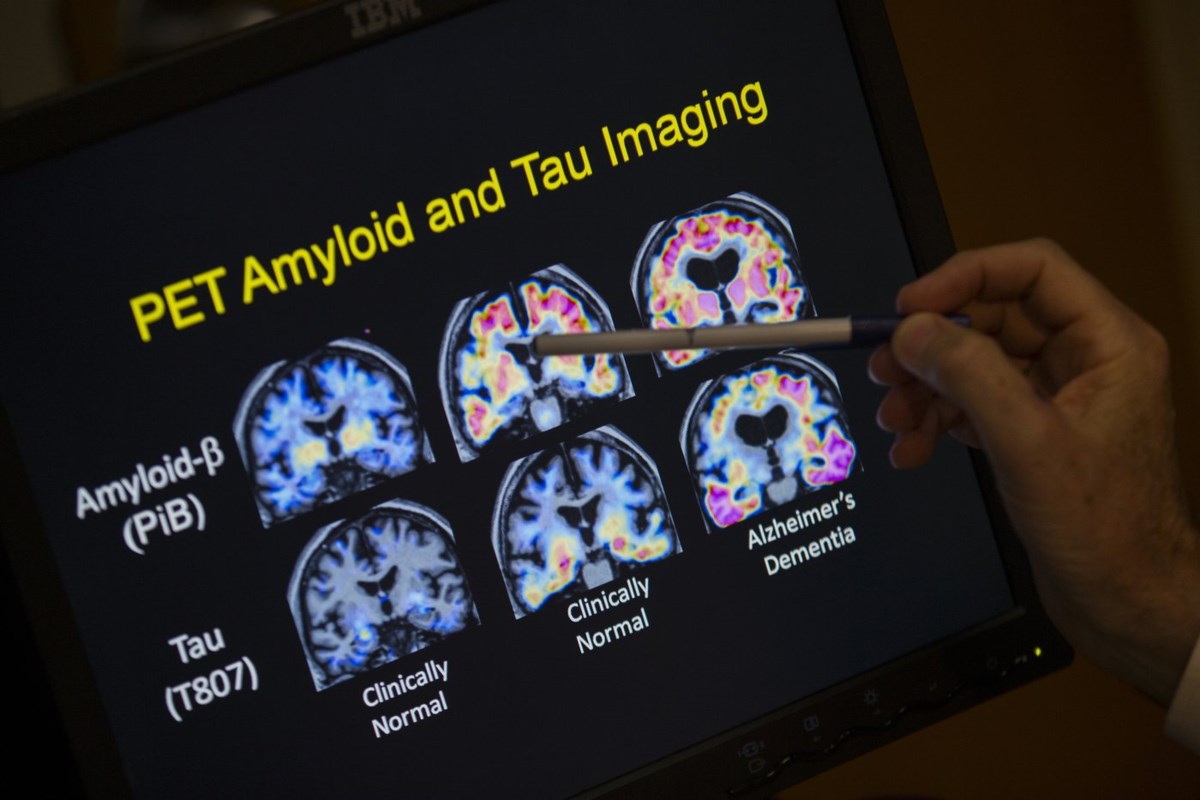
The test, developed by Fujirebio Diagnostics, Inc., works by identifying a sticky brain plaque known as beta-amyloid, which is a critical biomarker associated with Alzheimer’s. In the past, the only FDA-approved methods for detecting the presence of amyloid were either invasive spinal fluid tests or costly PET scans, which could be a barrier for many patients seeking accurate diagnosis.
One of the most significant implications of the approval of this blood test is its potential to make the diagnosis process more accessible and affordable. The lower costs and increased convenience of a blood test could lead to a wider usage of two new drugs, Leqembi and Kisunla, which have demonstrated their capacity to moderately slow down Alzheimer’s progression by clearing amyloid from the brain. Importantly, doctors are required to confirm the presence of amyloid in patients before prescribing these drugs, which necessitate regular intravenous infusions.
Dr. Michelle Tarver, a representative from the FDA’s center for devices, emphasized the importance of this new clearance, stating, “Today’s clearance is an important step for Alzheimer’s disease diagnosis, making it easier and potentially more accessible for U.S. patients earlier in the disease.”
In recent years, several specialty hospitals and laboratories have taken the initiative to develop their own in-house tests for amyloid. However, these tests have not undergone FDA review and typically lack insurance coverage. This situation has led to a landscape where healthcare providers have minimal reliable data to assess which tests are trustworthy and accurate, resulting in what some have referred to as a “wild west” of unregulated testing.
Moreover, a number of larger diagnostic and pharmaceutical companies are currently in the process of developing their own versions of blood tests aimed at receiving FDA approval. Companies such as Roche, Eli Lilly, and C2N Diagnostics are among those pursuing this goal.
It is important to note that these tests must be ordered by a licensed healthcare provider and are not intended for individuals who do not yet show any symptoms of Alzheimer’s disease.
___
AP Medical Writer Lauran Neergaard contributed to this story.
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
By Matthew Perrone, The Associated Press