The Importance of Sexual Health for Midlife British Women

In a revelation that might raise eyebrows or even lead to a collective yawn, a recent study from University College London has found that British women in midlife are experiencing a significant decline in sexual activity. As a women's health GP, I believe that this trend is concerning and warrants our attention. Women aged 55 to 64 report the least sexual activity compared to other age groups, a statistic that highlights an urgent issue within this demographic.
Factors contributing to this alarming trend include the myriad stresses that accompany midlife, such as the demands of motherhood, bustling careers, responsibilities towards aging parents, and the myriad challenges presented by menopause. Symptoms ranging from hot flashes to mood swings can understandably push sexual intimacy down the priority list for many. However, I contend that this is a grave oversight, as engaging in sexual activity plays a vital role in our overall health, particularly as we age.
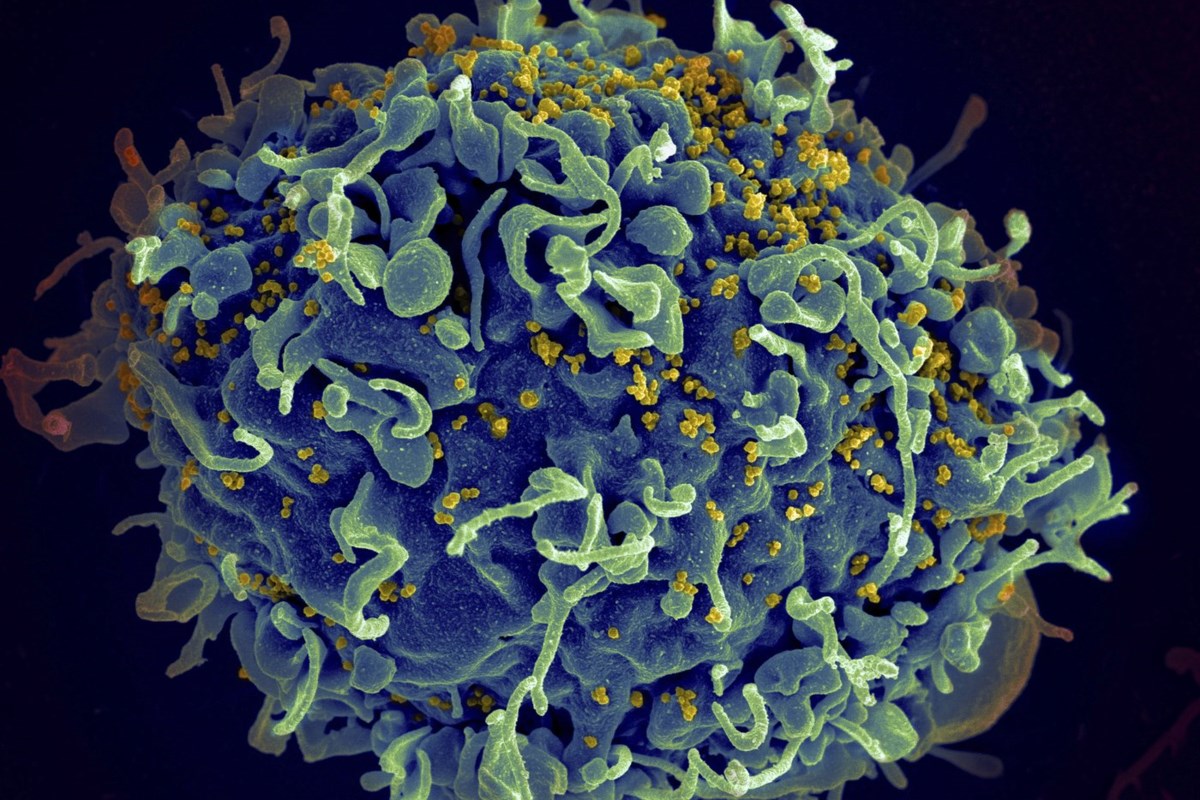
Research has consistently shown that sexual activity, irrespective of whether it culminates in penetration, has numerous health benefits. Engaging in sexual activities and experiencing orgasms can help lower blood pressure, relieve headaches, improve sleep quality, and alleviate stress. In fact, a recent study indicated that regular sexual activity may even reduce menopause symptoms, acting almost like a natural form of hormone replacement therapy.
Among the over 900 women surveyed in this study, those who engaged in regular sexual activity—defined as having intercourse within the last three months—reported fewer issues like vulval itching, pain, and dryness. This increase in sexual activity is thought to enhance blood flow to the genital area, which promotes tissue health and elasticity, as well as improves lymphatic circulation.
In a related discussion, acclaimed actress Dame Emma Thompson recently advocated for the inclusion of sexual health services within the National Health Service (NHS). Having played a character in the film Good Luck To You, Leo Grande—who hires a younger male sex worker—Thompson argued passionately that sexual health should be regarded with the same seriousness as any other aspect of our health.
As a 45-year-old mother of two teenagers and someone who has navigated the challenges of cancer treatment, I fully empathize with the hurdles faced by women at this life stage. The changes our bodies undergo during midlife can be daunting. Factors such as childbirth, hormonal fluctuations, and the natural aging process can complicate sexual experiences. Issues like diminished libido, aching joints, back pain, and the burdens of daily life can leave many feeling disheartened. However, it’s essential to remember that there are solutions and treatments available to help improve our sexual experiences.
For many in midlife, health challenges can diminish the appeal of sexual intimacy. Chronic pain, hormonal imbalances, stress, and sleep deprivation can all take their toll. If sex feels daunting or painful, it’s crucial to consult a healthcare professional. Many medical practices have female doctors specializing in women’s health who can provide tailored advice.
It’s also important not to dismiss genital discomfort or itching as merely a case of thrush. Conditions like lichen sclerosus, which leads to thinning and inflammation of the vulval skin, can require specific treatments. Addressing these matters with a doctor is critical for ensuring both comfort and sexual health.
Moreover, intimacy is not solely defined by penetrative sex. Physical touch through cuddling, massage, and affectionate gestures can all yield health benefits and strengthen emotional connections.
Hormonal changes during perimenopause and menopause can also substantially affect libido. Fluctuations in hormone levels can alter the time it takes to reach sexual arousal and affect the intensity of orgasms. Hormone Replacement Therapy (HRT), which increases estrogen levels, can alleviate many of these symptoms, including low sex drive. If HRT alone does not resolve libido concerns, additional testosterone prescriptions may be an option.
It’s critical to acknowledge that psychological factors, such as anxiety and depression, often contribute to diminished sexual desire. These issues can be addressed through various forms of therapy, including antidepressants and counseling, which may also help improve libido for some individuals.
Furthermore, for women experiencing discomfort during intercourse due to menopause-related symptoms, there are many options available to alleviate pain. Vaginal estrogen treatments, such as creams and gels, can significantly improve symptoms of genitourinary syndrome of menopause (GSM), which affects over half of all women in this age group. These products are safe for use even in those who have had breast cancer, although it’s essential to consult with a healthcare provider beforehand.
Lubricants also play a crucial role in enhancing sexual comfort, especially during menopause when natural lubrication decreases. There are various types of lubricants available, including water-based, oil-based, and silicone-based options, each with unique characteristics that can cater to individual preferences.
Additionally, many women may hesitate to use sex toys due to misconceptions about their implications for sexual health and relationships. In reality, these devices can be beneficial, enhancing sexual pleasure, increasing blood flow, and facilitating orgasms, thereby improving overall genital health.
Moreover, integrating sexual activity into one’s routine can help maintain a healthy sex life. As sexual arousal may shift from spontaneous to responsive during menopause, intentionally scheduling time for intimacy can foster stronger connections and enhance overall enjoyment.
In conclusion, the interplay of physical and psychological factors governing one’s sexual health can be complex and often intertwined. Seeking help from professionals specializing in this field can provide both partners the opportunity to explore new avenues for intimacy. Ultimately, sex can be a vital component of health, and prioritizing it—even amidst the challenges of midlife—can lead to a more fulfilling quality of life.
As Suzanne Noble, who hosts the podcast Sex Advice For Seniors, states, discovering vaginal estrogen transformed her sexual experience after menopause, allowing her to enjoy intimacy without pain. Her journey underscores the importance of being proactive about sexual health and exploring options that can enhance one’s quality of life.