Living with Crohn’s: A Galwaywoman’s journey of hope and the fight for awareness

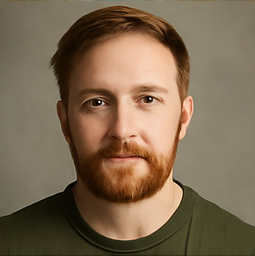
For Rebecca Hogan, life took an unexpected turn in October 2019. The 27-year-old from Clarinbridge had always been active, full of plans for the future, when her body began sending her distress signals that she could no longer ignore. “From around May 2019, I noticed an increase in stomach pains and the frequency of going to the bathroom,” Rebecca recalls. Initially, her GP prescribed medication, but when the symptoms worsened — with alarming weight loss and increasing weakness — a referral to a consultant followed. A colonoscopy confirmed the diagnosis: Crohn’s disease, a form of inflammatory bowel disease (IBD ). “I didn’t take it well initially,” Rebecca admits. “The thoughts of a lifelong condition and taking injections really upset me. I worried about how the life I had all planned out in my head was going to change.” Crohn’s disease, alongside ulcerative colitis, falls under the umbrella of IBD, affecting an estimated 50,000 people across Ireland. With Crohn’s, inflammation can strike anywhere along the digestive tract, causing debilitating symptoms such as urgent bowel motions, stomach cramps, painful joints, and skin rashes. Despite ongoing research, the exact causes remain elusive, with genetics, diet, gut bacteria, and environmental factors all implicated. Rebecca’s early experience is one shared by many who face a chronic diagnosis: fear, uncertainty, and grief for the life they imagined. However, her story did not end there. With resilience and the right support, she gradually adapted to her “new normal.” “Today, while there are still tough days, all in all, I am a lot better than I have ever been,” she says. “I don’t take things for granted anymore.” Rebecca credits her support network — her husband Liam, her family, and her friends — alongside a flexible, understanding employer who allowed her to work from home, greatly reducing the anxiety that often accompanies chronic illness. Importantly, Rebecca’s journey is also marked by joyful milestones: her wedding day in June 2022, a dream trip to New York in 2023, and most recently, a pregnancy she once feared might never happen. “I am truly blessed,” she shares. “I remember lying in a hospital bed in 2021, wondering if all this would ever be possible. I share my story because, had I read something like this back then, it would have given me hope — and I would love to give that hope to someone else.” Beyond What You Can See: The Hidden Realities of Crohn’s Rebecca’s story underscores a vital point: the invisible nature of IBD. “Just because someone doesn’t look sick doesn’t mean that they aren’t,” she emphasises. Many people living with IBD suffer in silence, dealing with fatigue, brain fog, and anxiety on top of their physical symptoms. Because of this, misconceptions can easily arise, leading to hurtful remarks, even if unintentional. Phrases like “You look fine — are you sure you’re that sick?” are all too common. To tackle this issue head-on, Crohn’s and Colitis Ireland is launching a major new initiative: the Gut to Know conversation guide. Designed to improve how we talk to and support those with IBD, the guide aims to foster empathy and understanding, highlighting how better conversations can ease emotional burdens. As part of this awareness campaign, a special free webinar, IBD 101, will be held on Monday, May 19, from 6.30pm to 8.30pm. This webinar promises a deep dive into the realities of living with IBD, providing insights for patients, families, friends, and health professionals alike. IBD 101: A Vital Conversation for Change The upcoming webinar will bring together a host of expert voices and personal testimonies. Consultant gastroenterologist Professor Anthony O’Connor of Tallaght University Hospital will offer a comprehensive introduction to IBD — from symptoms and diagnosis to treatment and coping strategies. Joining him will be psychologist Dr Jennifer Wilson O’Raghallaigh, who will explore the emotional dimensions of living with chronic illness, including how loved ones can best offer support. “Most of the time, loved ones feel compassion but don’t know exactly how to express it,” Dr Wilson O’Raghallaigh explains. “Good communication strategies, like those in the Gut to Know guide, can help navigate tricky conversations and enable family and friends to better offer support.” Also sharing their personal stories during the webinar will be Armagh GAA star Niall Grimley and Gogglebox Ireland TV critic Sarah Reilly. Both live with IBD and will recount their own experiences of conversations — both helpful and harmful — with friends, family, and the wider community. The free webinar, supported by Pharmacosmos, is open for registration at www.crohnscolitis.ie The number of people living with IBD in Ireland is significant — and growing. With no known cure, managing IBD is about symptom control, flare-up prevention, and maintaining the best possible quality of life. Treatment often involves medication to suppress inflammation, lifestyle adjustments, and sometimes surgery. Lifestyle factors play an important role too. A healthy, balanced diet, avoiding smoking, moderating alcohol intake, and managing stress levels can make a significant difference. Yet, even with the best strategies, IBD remains unpredictable, and flare-ups can occur without warning. Support networks like Crohn’s and Colitis Ireland are crucial in this landscape, offering education, community, and direct help through their Support Line (01 531 2983, open Mon/Wed/Fri, 9.30am–12.30pm ) and online resources. For Rebecca, volunteering with the organisation is a way to give back and stay connected to a community that understands. She is also passionate about baking, cooking, and spending cherished time with her goddaughters Victoria and Olivia — enjoying every small moment that once seemed so out of reach. Rebecca’s story — and the broader campaign around Gut to Know — brings to light an important truth: language matters. When facing a chronic illness, the difference between feeling supported and feeling isolated can sometimes hinge on a few simple words. As Dr Wilson O’Raghallaigh notes, chronic illness doesn’t just affect the person diagnosed; it shifts the lives of everyone around them. “Family members and friends are embarking on a journey of health discovery too,” she says. “There are learnings for everyone.” By embracing better conversations, by really listening rather than assuming, we can create a kinder world for people living with IBD — and for everyone managing invisible illnesses. In the end, Rebecca Hogan’s story is not just one of illness — it is one of resilience, growth, and hope. Her life today, filled with love, purpose, and new beginnings, stands as a testament to what is possible even in the face of daunting odds. “I want people who are struggling to know that better days are possible,” she says. “You are more than your diagnosis. You are still you — and there are still so many wonderful things ahead.” Six Tips for Talking to People with IBD about IBD Privacy please. Ask the person with IBD if it’s OK to ask questions about their condition. Some may be happy to talk. Others may not. Listening and offering your undivided attention helps the person to feel supported. Ask open-ended questions such as “how are you feeling today?” Offer empathy not pity. Acknowledge the person’s feelings and circumstances but avoid expressing pity. “I’m here for you” or “is there anything I can do?” are so much more helpful than “I feel so sorry for you”. Acknowledging unseen symptoms such as fatigue, joint pain and mental stress with the words “I believe you” can provide great comfort and relief. Think before you speak. Avoid blaming the person or trivialising what they are going through. Saying “you’re stressing too much” or “everyone gets stomach aches” or “I heard about a miracle cure” do nothing to improve their situation. Getting down to business. If you’re an employer, are there ways in which you can adjust workloads, or provide for flexible hours, breaks or remote working, that would help your colleague? Think about the work environment and how accessible the toilet facilities are. Let your colleague know that it’s safe to discuss their needs without fear of judgement—“I want to sit down with you to find solutions that work for everyone”. School of life. If you’re a teacher, allow the student to leave the class without having to ask for permission. For example, you could say “If you need to leave class, just go, we’ll catch you up later”. Think about how school deadlines can be adapted in the event of absence due to a flare-up. If going on a school trip, consider how the student can travel in comfort and enjoy the activity. Collaborate with the school counsellor to ensure emotional support is available as required. A shoulder to lean on. If you’re a family member or friend, do include the person with IBD on invites to nights out and outings, but if the person is unwell and the answer is “no”, respect that. For example, you could ask “Would you like to stay in or do something low-key if you’re not up to going out?” Offer practical help with chores, errands and travel to medical appointments. On more manageable days, celebrate “small wins” and enjoy the moment.