Understanding Male Infertility: The Challenges Faced by Pediatric Cancer Survivors

Nivan's story is a poignant reminder that he is not alone in facing the challenges of infertility. Recent studies indicate that up to two-thirds of male pediatric cancer survivors encounter infertility as they move into adulthood. The primary culprits behind this heartbreaking reality are radiation and chemotherapy treatments, which can lead to a severe form of male infertility known as non-obstructive azoospermia (NOA). This condition is characterized by the body producing very few, if any, sperm at all.
Infertility, while rarely discussed openly, is a significant issue affecting many men. In fact, it is estimated that NOA impacts approximately one in every 100 men, including individuals of diverse gender identities who were assigned male at birth. The emotional toll of infertility can be particularly devastating for both men and couples who wish to conceive. Dr. Flannigan, an associate professor and director of the Reproduction and Sexual Medicine Centre in the UBC Department of Urological Sciences, shares, “Infertility can be really, really difficult for a lot of men and couples that I see. It takes an emotional toll.”
Globally, the landscape of infertility is alarming, with about one in six couples struggling to conceive. Interestingly, around half of these cases can be attributed to male infertility factors, including NOA, which is estimated to affect about 15 percent of men diagnosed with infertility. The causes of NOA can range from the aftermath of cancer treatments to various genetic conditions. However, in the majority of cases, the specific underlying cause remains a mystery. This uncertainty drives Dr. Flannigan and his colleagues to leverage next-generation bioengineering, genomics, and machine-learning technologies in their quest to uncover the roots of this condition.
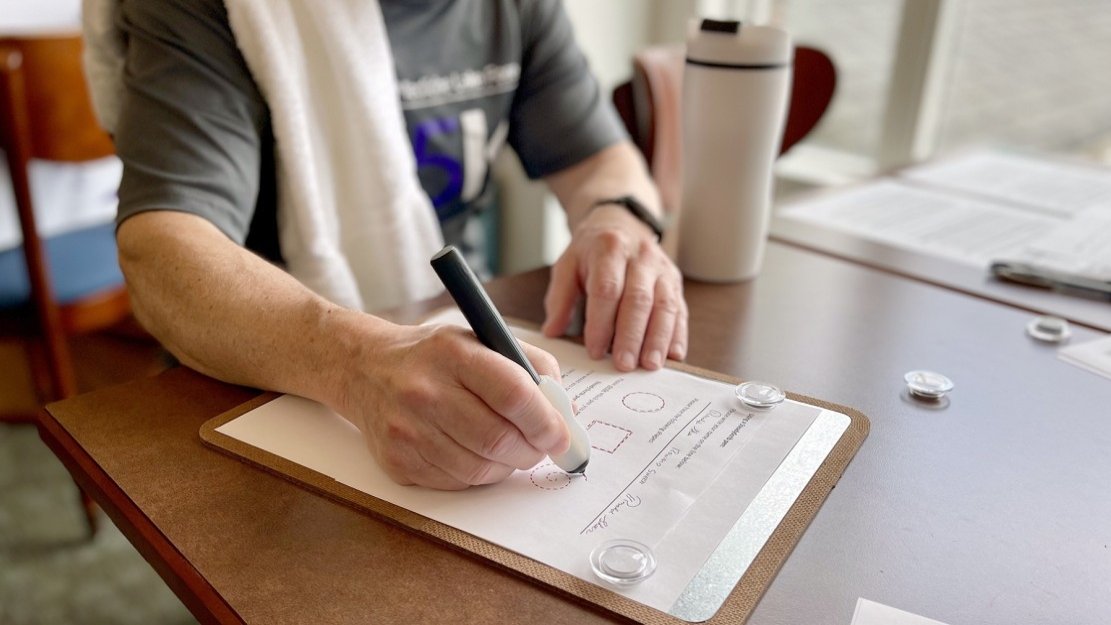
As for treatment, the current options available for patients diagnosed with NOA are quite limited. The only available remedy is an invasive and time-consuming procedure that involves surgically extracting testicular tissue to search for ‘rare sperm.’ Dr. Flannigan elaborates on the intricacies of this challenging process, stating, “If we find enough viable sperm, we can do IVF. Right now, we’re able to find sperm about 50 percent of the time, but that doesn’t guarantee success. We ideally need to find at least one sperm per each egg, among millions of other cells, which takes hours. It’s the literal definition of looking for a needle in a haystack.” This highlights not only the complexity of infertility treatment but also the urgent need for advancements in medical technology to assist those affected.