Revolutionizing Diabetes Management: New Tools Enhance Blood Sugar Prediction While Safeguarding Privacy

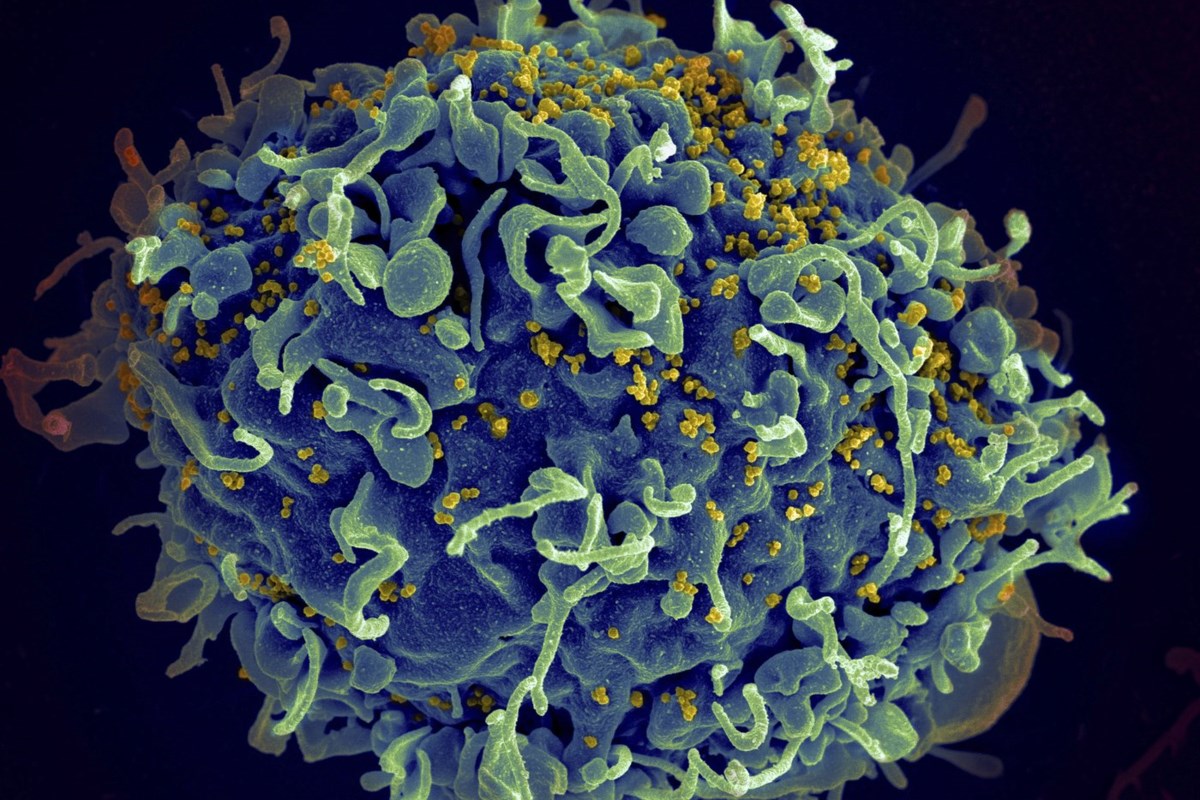
Managing diabetes is a daily challenge confronted by nearly 40 million Americans, a statistic highlighting the significant impact of this chronic condition on a large segment of the population. Individuals living with diabetes must continuously monitor their food intake, manage their medication schedules, and engage in regular physical activity. Errors in any of these aspects can lead to severe health complications, underlining the critical need for more sophisticated prediction tools that enhance diabetes care.
To improve diabetes management, a team of researchers, supported by multiple grants from the U.S. National Science Foundation, is pioneering innovative tools designed to help patients forecast their blood sugar levels with greater accuracy. Importantly, these developments prioritize patient privacy, ensuring that sensitive health data remains secure. This groundbreaking approach has the potential to significantly alter the landscape of diabetes monitoring and self-management, allowing individuals to gain real-time insights into their health.
The foundation of this advanced technology is a method called federated learning. This technique enables artificial intelligence models to be trained across numerous patients' devices without the need to transmit any personal data to a central server. This decentralized approach is particularly well-suited for healthcare environments where data privacy is of utmost importance. Additionally, it is tailored to accommodate the limitations of battery life and memory capacity present in many smart devices used by patients. However, initial federated learning systems faced challenges in adapting to individual variations, such as differing dietary habits, exercise routines, and responses to insulin.
To overcome these hurdles, the research team devised a strategy to categorize patients based on their carbohydrate intake levels—including sugars and starches. The rationale behind this method is that individuals with similar eating patterns are likely to exhibit comparable glucose response patterns. By training the AI on these grouped behaviors, the model became more adept at making personalized predictions regarding blood glucose levels.
In order to validate their approach, the researchers assessed two machine learning models using data produced from an FDA-approved Type 1 diabetes simulator. As the simulated data grew, the accuracy of the models also improved. Remarkably, the system was able to construct personalized models even with limited input data—an essential benefit for newly diagnosed patients or those who are just beginning to incorporate digital tools into their management strategies.
Conventional AI systems typically necessitate the collection of vast quantities of data in a centralized format, which raises privacy concerns, especially when it pertains to sensitive health information. Federated learning, in contrast, resolves these issues by retaining personal data within each individual's device—such as smartphones or wearable sensors—and exclusively sharing the model's learning outcomes, without ever disclosing the raw data. This not only protects patient privacy but also facilitates continuous improvement of the system over time.
While the initial findings are promising, the research team acknowledges that the models still depend heavily on meticulous food intake data, a requirement that not all patients can fulfill easily. Therefore, they intend to broaden their system to account for additional factors such as physical activity and medication use, along with plans to test it within larger patient cohorts. Ultimately, the researchers aspire to extend this personalized, privacy-conscious AI approach to address other chronic conditions, such as heart disease or asthma, where tailored care is equally crucial.
Given that diabetes incurs a staggering cost of over $300 billion annually to the U.S. economy, advancements that facilitate earlier intervention and personalized care have the potential to reduce long-term expenses while enhancing health outcomes across the population.
This project serves as a compelling example of how public investment in cutting-edge research can propel innovations that not only benefit individual patients but also strengthen the entire U.S. healthcare system.