Unveiling the Role of Olfactory Ensheathing Cells in Spinal Cord Injury Repair
Olfactory sensory neurons (OSNs) are truly fascinating due to their unique ability to undergo neurogenesis throughout an individuals life within the adult olfactory epithelium. This remarkable discovery, first noted by Graziadei and Monti Graziadei in 1985, highlights the adaptability and resilience of these neurons. The axons of these OSNs have a specialized relationship with a particular type of glial cell known as olfactory ensheathing cells (OECs), initially described by Doucette in 1990. OECs play a crucial role in guiding the growth of OSN axons towards their designated glomerular targets, and they exhibit impressive regenerative abilities when faced with injury. This has led to significant interest in OECs and their potential applications in treating spinal cord injuries (SCIs).
The regenerative capacity of adult spinal cord neurons is notably hampered by the environment at the lesion site. This environment includes a reactive glial scar, along with infiltrating meningeal fibroblasts and various immune cells, which collectively create a challenging barrier for axonal regeneration. According to research conducted by Burda and Sofroniew in 2014 and Wanner et al. in 2013, the lesion core primarily consists of non-neural tissue that actively inhibits axonal outgrowth. This inhibition occurs due to the upregulation and secretion of chondroitin sulfate proteoglycans, which are known to block the regeneration of axons.
In studies involving severe or complete spinal cord transection in rats, the transplantation of OECs has shown promising outcomes. These studies have demonstrated that OECs can surround axon bundles, facilitating regeneration into and even across the injury site. Research conducted by Khankan et al. in 2016, Ramn-Cueto et al. in 2000, and Takeoka et al. in 2011 has further supported this notion. In combination with in vitro studies, detailed examinations of injury sites have suggested that OECs serve multiple functions: they act as phagocytes to eliminate degenerating axonal debris and necrotic cells, modulate the immune response to injury, and interact positively with the glial scar and lesion core formed after injury.
OEC transplantation has been found to create an environment conducive to neural repair, as evidenced in studies by Khankan et al. in 2016 and Takeoka et al. in 2011. These cells secrete various molecules such as Brain-derived neurotrophic factor (Bdnf), Nerve growth factor (Ngf), and Laminin, all of which stimulate axon outgrowth. Notably, research by Windus et al. in 2007 revealed that OECs enhance cell-to-cell interactions between neurites and themselves even in inhospitable environments. In a 2015 study, Khankan et al. discovered that neurites grown in growth-inhibitory areas of multicellular cultures exhibited two to three times more growth when associated with olfactory bulb-derived OECs (OB-OECs).
The outcomes of OEC transplantation in the context of spinal cord injuries (SCI) have varied widely across the literature, largely due to the technical differences in experimental designs. The origin of OECs plays a significant role in these outcomes, with studies indicating that OB-OECs tend to be more effective than those derived from the lamina propria. Furthermore, the timing of OEC transplantationwhether acute or delayedalong with the severity of the injury (ranging from hemisection to complete spinal cord transection) and the age of the injured host, all significantly influence results. A comprehensive evaluation by Franssen et al. in 2007 found that out of 56 studies on OEC transplantation, 41 demonstrated positive effects, including the stimulation of regeneration and beneficial interactions with the glial scar.
In a collaborative research effort, we conducted six studies involving SCI in adult rats, utilizing a model of completely transected thoracic spinal cord followed by OB-OEC transplantation. Results from five of these studies provided compelling physiological and anatomical evidence of axonal regeneration into and across the injury site. Takeoka et al. in 2011 reported notable physiological evidence of motor connectivity across the transection in rats treated with OECs, unlike in control groups receiving media alone. This was achieved through transcranial electric stimulation of the motor cortex or brainstem, which detected motor-evoked potentials (MEPs) in hindlimb muscles at four and seven months post-transection. Remarkably, after seven months, 70% of the OEC-treated rats exhibited responses to stimulation.
A follow-up re-transection above the original transection site eliminated all MEPs in the OEC-treated rats, providing strong evidence of axonal conductivity across the injury site. Furthermore, three long-term studies assessed the anatomical axonal outgrowth of the descending serotonergic Raphespinal pathway. The results showed that significantly more serotonergic-labeled axons crossed the rostral inhibitory scar border and occupied a larger area within the injury core in rats that received OEC transplants compared to controls.
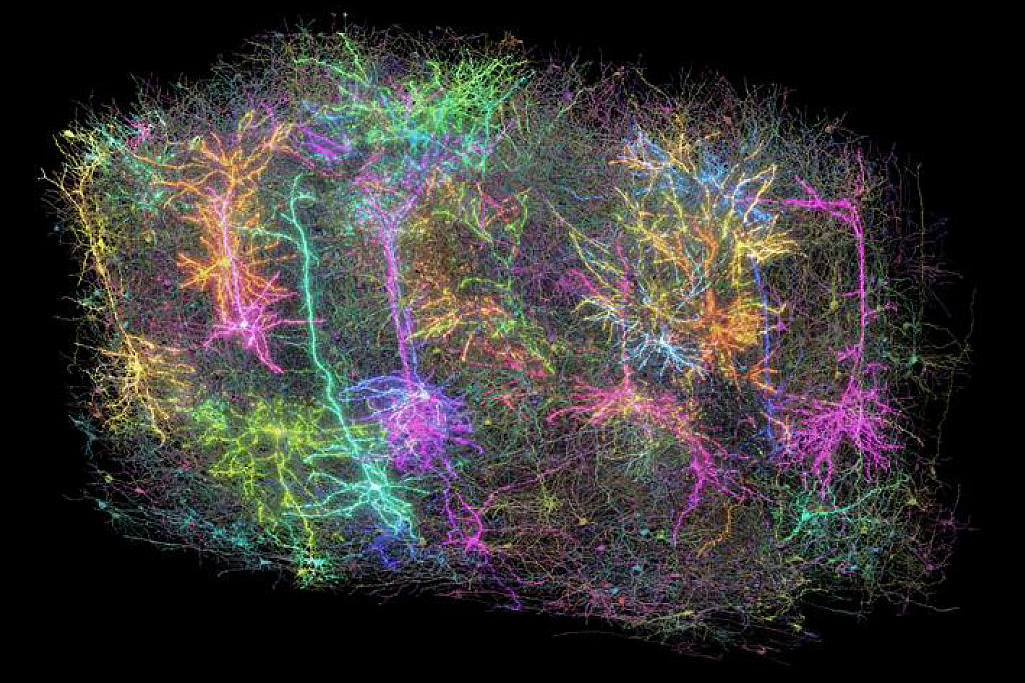
The current study aims to investigate how OB-OECs execute the various functions associated with neural repair. We hypothesize that distinct OB-OEC subtypes exist, each with unique gene programs and secreted molecules that contribute to their reparative activities. By employing single-cell RNA sequencing (scRNA-seq), we have characterized the immunopurified female rat OB-OECs, analogous to those transplanted in previous studies. Our analysis revealed five distinct OEC subtypes, each expressing unique marker genes, further confirmed through experimental approaches. Additionally, we explored key extracellular matrix (ECM) molecules secreted by OECs, such as Reelin (Reln) and Connective Tissue Growth Factor (Ccn2/Ctgf), which may play a critical role in facilitating axonal outgrowth within the challenging environment of the injury core.