Unveiling the Role of Microglia Aging in Cognitive Decline
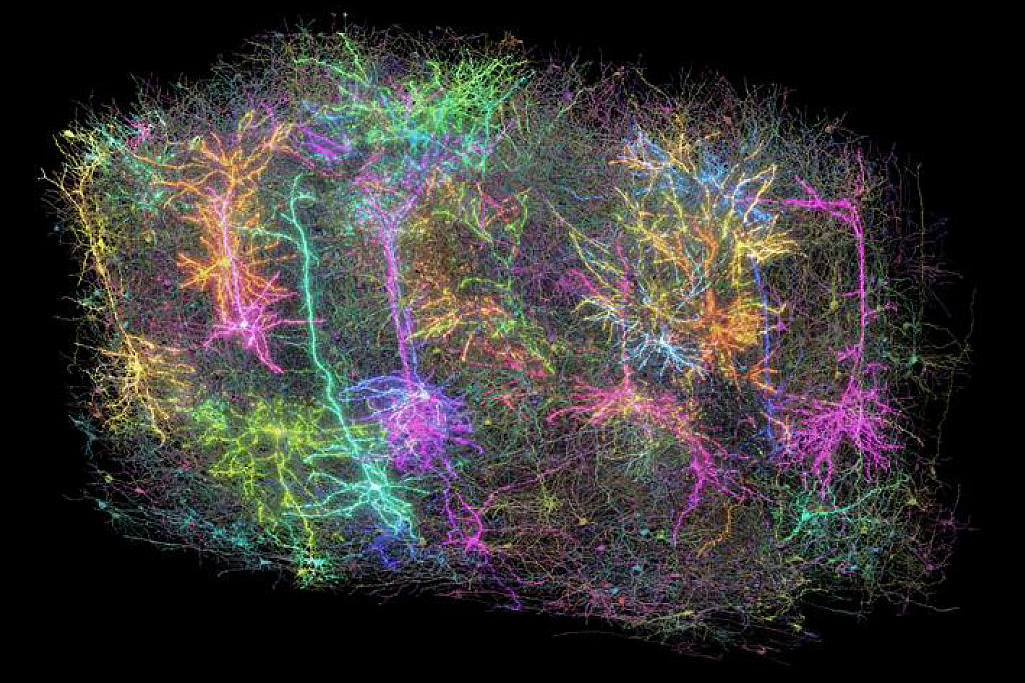
Recent research has made significant strides in understanding how the aging of microglia in the hippocampus can lead to cognitive decline associated with age. Microglia, the brain's resident immune cells, undergo a series of intermediate changes as they age, transitioning through states that precede inflammatory activation. This process not only contributes to the aging process itself but also has profound implications for cognitive health as we grow older.
The study highlights that these intermediate states, which include the activation of stress response pathways and the TGF signaling mechanisms, act as important modulators for further age-related inflammatory activation. Interestingly, the research reveals that microglia display variations in their aging progression across different regions of the hippocampus, suggesting that their responses are closely tied to the systemic environment and the presence of neurodegenerative diseases.
Through the analysis of single-cell RNA sequencing (scRNA-Seq) data, the researchers uncovered critical, albeit hidden, intermediate states that microglia experience as they transition towards an inflammatory activation linked to aging. These states have been observed in middle-aged mice and are part of the stress-response pathways that likely respond to various internal and external cellular stressors.
The pseudotime analysis conducted in the study offers a plausible sequence of molecular changes leading to age-related inflammatory activation within hippocampal microglia. The process starts with mitochondrial dysfunction, which initiates a stress response, producing components like TGFB1 that aim to restore microglial homeostasis. However, chronic stress response activation can lead to an enhanced translational capacity, further promoting inflammatory activation. Notably, this inflammatory activation can progress independently of increased translational capacity, as evidenced by experimental results showing that inhibiting translation did not significantly affect microglial activation following stimulation with lipopolysaccharides (LPS).
Additionally, the study found that intermediate states of microglial aging were also evident in young adult heterochronic parabionts, underscoring the influential role of the aged systemic environment in driving microglial progression toward inflammatory activation. While the researchers noted signs of early inflammatory activation in the hippocampus by the age of 12 months, consistent with observations in whole-brain analyses, they acknowledged that scRNA-Seq analysis did not reveal such intermediate stages in the entire brain. This discrepancy may stem from the examination of multiple regions with distinct transcriptional programs, which could obscure regional aging trajectories.
The research emphasizes the necessity for both temporal and regional specificity in aging studies, especially given the cellular diversity observed across different ages and brain regions. Within the hippocampus, the local microenvironment significantly influences microglial aging; variations in cellular function and composition across different subregions yield different outcomes as microglia age and respond to an aged systemic environment. The accumulation of activated microglia in various hippocampal subregions begins around 12 months of age, indicating that age-related changes are present much earlier than previously believed.
Interestingly, the study identified that the inflammatory trajectory of microglial aging could be mitigated in vitro through TGF signaling. Conversely, the absence of microglia-derived TGFB1 accelerated the progression along these aging-associated inflammatory pathways in vivo. This suggests that TGF signaling is crucial for maintaining a youthful state in microglia and plays a key role in managing the advancement along aging-associated inflammatory trajectories.
Moreover, the results reveal that a loss of microglia-derived TGFB1 led to cognitive impairments dependent on age, hinting that progression through these inflammatory pathways might significantly contribute to cognitive decline as people age. Given that a brief surge in Tgfb1 expression is observed in middle-aged microglia, it raises the possibility that sustaining this stress response-mediated signaling into older ages could help delay microglial dysfunction and preserve cognitive function.
While microglia are known to facilitate cognitive function during brain development and are also implicated in neurodegeneration, the understanding of how age-related changes in microglia influence cognitive performance remains limited. The specific deficits noted in Tgfb1 heterozygous and conditional knockout mice suggest that the age-related alterations in microglia-derived TGFB1 predominantly affect hippocampal-dependent cognitive decline.
In conclusion, this research underscores the importance of studying aging in a region-specific manner to uncover crucial cellular intermediates involved in the aging process. With its focus on microglia, the findings have broader implications for other research that seeks to determine how aging-related changes affect various cell types within the hippocampus. Therapeutic strategies aimed at targeting these intermediate states during aging could prove to be pivotal in combating age-related pathologies, particularly those that contribute to cognitive dysfunction.