Tufts Researchers Develop Next-Gen Weight Loss Drug Targeting Multiple Hormones

In the United States, weight loss drugs such as Ozempic and Wegovy have emerged as popular options for over 15 million adults, which accounts for approximately 4.5% of the population. Although these medications have proven effective in aiding weight loss and managing blood sugar levels, they come with a set of drawbacks that have raised concerns among users and healthcare providers alike. Reports indicate that the weight loss effects may diminish once the treatment is discontinued, and potential side effects, including osteoporosis and muscle loss, have sparked discussions about the long-term risks associated with these drugs. Additionally, many users experience nausea, which can make it challenging to adhere to the treatment plan.
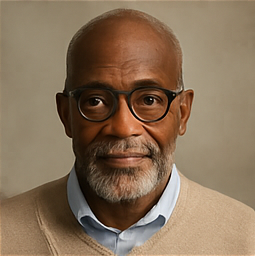
In response to these issues, a team of researchers at Tufts University, led by Krishna Kumar, the Robinson Professor of Chemistry, has developed a new, next-generation compound aimed at improving effectiveness while reducing side effects. Their findings were published in a recent paper in the Journal of the American Chemical Society.
The existing weight loss drugs currently available in the market primarily target one, two, or at most three hormone receptors that are involved in glucose metabolism and appetite regulation. However, the Tufts research team has identified a crucial fourth target that could enhance the overall efficacy of weight management strategies. “Obesity is linked to over 180 different health conditions, including cancer, cardiovascular disease, osteoarthritis, liver disease, and type 2 diabetes, affecting over 650 million individuals globally,” Kumar explained. “Our motivation stems from the aspiration to develop a single drug capable of treating obesity while simultaneously reducing the risk of these numerous health complications.”
Understanding Hormonal Mechanisms
After consuming food, our bodies initiate a hormonal “fuel gauge” system that regulates glucose levels and signals when we have eaten enough. One of the key hormones involved in this process is glucagon-like peptide 1 (GLP-1), which is responsible for stimulating insulin production and facilitating glucose uptake by muscle and other tissues. When glucose is effectively absorbed by the cells, blood sugar levels return to normal. Ozempic enhances GLP-1's effectiveness through minor modifications to ensure its increased availability in the bloodstream. As a result of its success in managing blood glucose, the American Diabetes Association has recommended it, along with other GLP-1-based medications, as the premier injectable treatment option for diabetes, surpassing insulin itself.
Moreover, GLP-1’s role extends beyond metabolism; it also acts on the brain to promote feelings of fullness after meals and slows gastric emptying, allowing for a more gradual release of nutrients and glucose into the bloodstream. This dual functionality has contributed to its rising popularity as a weight loss treatment.
Despite its benefits, GLP-1 drugs are not without flaws. “The most significant challenge associated with GLP-1 medications is the necessity of weekly injections, accompanied by instances of severe nausea,” Kumar noted. “Statistics reveal that nearly 40% of individuals using these drugs discontinue treatment within the first month due to these adverse effects.”
A second hormone, glucose-dependent insulinotropic peptide (GIP), is also released during meals, contributing to feelings of satiety. Given the structural similarities between GLP-1 and GIP, researchers have developed a combined peptide that integrates features from both hormones, referred to as a chimera. This novel drug, marketed as Mounjaro or Zepbound (the brand names for tirzepatide), has demonstrated a significant reduction in nausea, rendering it a more tolerable option that could potentially surpass Ozempic in the weight loss arena.
Kumar elaborated further, “There exists a third hormone—glucagon—that, counterintuitively, elevates blood glucose levels while also increasing cellular energy expenditure, raising body temperature, and suppressing appetite.” By incorporating glucagon into the mix, the GLP-1 and GIP hormones can counteract its glucose-raising effects while capitalizing on their complementary functionalities to enhance weight loss outcomes.
Glucagon shares structural similarities with both GLP-1 and GIP, prompting drug developers to create a single chimera peptide that can activate receptors for all three hormones. This innovative drug, named retatrudide, is currently undergoing clinical trials and has shown promising results, indicating potential weight loss of up to 24%, significantly higher than the 6-15% weight reduction typically associated with existing GLP-1 drugs.
Aiming for the Gold Standard in Weight Loss Solutions
Kumar remarked, “The ultimate goal in the fight against obesity is achieving outcomes comparable to those of bariatric surgery, a procedure that effectively reduces stomach size and can lead to substantial, lasting weight loss—up to 30%.” For many individuals grappling with chronic obesity and its associated health risks, such surgical interventions may become not just preferred but necessary due to their invasive nature.
While current injectable weight loss medications have yet to reach this benchmark, the Tufts chemists are dedicated to redesigning drug formulations that could match the impressive results of bariatric surgery.
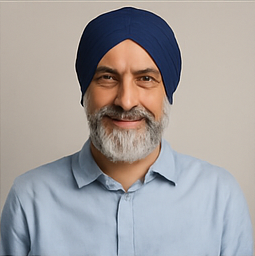
“We aimed to incorporate one more hormone into our therapeutic arsenal to complete the quartet of weight management,” stated Tristan Dinsmore, a graduate student in Kumar’s lab and the study's lead author. “This crucial hormone is peptide YY (PYY), which is also released by the gut post-meal, and is known for its appetite-suppressing effects while slowing gastric emptying through distinct mechanisms compared to GLP-1 or GIP. PYY may also contribute to fat burning.”
As PYY belongs to a different and structurally unrelated class of hormones than the initial trio, combining its structure into a chimeric peptide alongside GLP-1, GIP, and glucagon posed challenges. Nevertheless, the Tufts research team succeeded in linking two peptide segments end-to-end to create a novel ‘tetra-functional’ clinical candidate.
“One limitation faced by current medications is the individual variability in how patients respond to hormones and express target receptors, which often results in suboptimal weight loss outcomes,” explained Martin Beinborn, a visiting scholar in the Department of Chemistry. “By targeting four distinct hormone receptors simultaneously, we aim to mitigate variability and enhance the likelihood of achieving better, more consistent effectiveness.”
Beinborn further noted, “Another issue is the tendency for patients to regain weight after stopping treatments involving GLP-1-related drugs. Thus, it’s essential that lifestyle modifications complement medication to support individuals in attaining and maintaining their target weight while preserving muscle and bone mass.”
“Recent studies suggest that weight regain may be postponed with newer, more effective GLP-1 mimetics,” he added. “Building on these observations, it is plausible that multi-chimeric designs, like the one we discovered, could bring us closer to the lasting weight loss standards established by bariatric surgery.”